Why Bloating Happens During Menopause and Perimenopause and What You Can Do About It
If you’ve noticed that bloating, constipation, or unpredictable digestion have become a regular part of life since hitting your 40s or 50s, you’re definitely not alone. Bloating during perimenopause and menopause is incredibly common, and for many women it can feel frustrating, uncomfortable, and sometimes even embarrassing.
Hormone fluctuations, stress, sleep changes, and a slowing digestive system can all contribute but the good news is that there are ways to manage it. As a dietitian with over 25 years of experience working with women through this stage of life, I’ve seen how the right nutrition and lifestyle changes can make a big difference.
In this guide, we’ll look at why bloating becomes more common during perimenopause and menopause, how factors like hormones and gut health are connected, and most importantly, the practical steps you can take to feel more comfortable and confident again.
In this article, you’ll discover:
- Why bloating is so common during perimenopause and menopause
- How hormones, stress, and sleep all play a role
- Practical dietitian-approved tips to ease symptoms and support gut health
Every week I receive at least one enquiry from a woman who is experiencing gut issues such as bloating, constipation, and diarrhoea. One question I always ask is how old they are and, depending on the answer, where they are on their menopausal journey. Often, they feel they are in perimenopause, or they’ve always struggled with digestive issues and have now reached menopause.
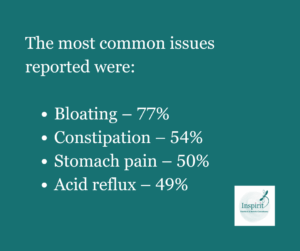
Although it’s a relatively unexplored field of medicine (women’s health in general is underfunded and under-researched), this is something many dietitians are seeing. A survey carried out by Dietitian Nigel Denby (1), asking 574 women aged 44–73 about their digestive issues, found that a whopping 94% reported experiencing digestive problems. Here’s what they found:
Why Bloating Gets Worse During Menopause and Perimenopause?
How Hormonal Changes Affect Digestion and Bloating
Fluctuating hormones can play havoc in many areas during this time. Although it’s a relatively new area of research, we do know that the gut microbiome plays a role in hormone regulation.
Simply put, oestrogen is produced and, once it has circulated in the bloodstream, it is taken to the liver, broken down, and mixed with bile to pass through your intestine and be excreted in your poo. We now know that certain bacteria in the gut can take this oestrogen, which was destined to be excreted and effectively recycle it, making it active once again. These bacteria are known as the estrobolome. There is evidence to support that this also happens with other sex hormones too. If you want to read more about it, reference 2 is for you.
We also know that declining hormone levels can lead to a reduction in the diversity of the gut microbiome.
The Hidden Role of Stress in Menopause Bloating
It is well known that stress plays a role in digestive issues such as bloating, constipation, and diarrhoea. Often, you enter perimenopause at the same time as navigating the teenage years with your children, caring for older relatives, or juggling a senior position in your career. At a time when you thought life would be getting easier, it often isn’t and you continue to put everyone else ahead of yourself.
This can result in increased adrenaline and cortisol levels and often leads to less beneficial lifestyle behaviours.
How Sleep Disruptions Contribute to Bloating During Menopause
Sleep is often a problem during perimenopause and menopause, whether it’s hot flushes, needing to get up to pee, or being wide awake at 3 am with everything running through your head. Science tells us that poor sleep affects the gut–brain connection, increases inflammation, and heightens sensitivity to pain.
My 25 years of experience as a dietitian tells me that sleep issues often lead to an increased reliance on caffeine and a poorly balanced diet with a larger proportion of processed foods, which are typically higher in fat and sugar.
7 ways to Reduce Bloating During Perimenopause and Menopause
Tackle Constipation: A Key Step to Reducing Bloating
Most of my clients who are suffering from bloating also have constipation. You can be constipated even if you go to the toilet every day! As you get older, your digestion can naturally slow down. It can also be affected by changes in hormones, stress, and activity levels. I would also say that, in most post-menopausal women I see, constipation and bloating are the predominant gut issues.
While we often associate anxiety with causing us to rush to the bathroom, in menopausal and post-menopausal women I often see it causing constipation instead.
Here’s what to look out for to determine if you might be constipated:
- If you have to strain
- If you pass small poos like rabbit droppings or dry, cracked stools
- If you go for a poo but feel that you haven’t fully emptied your bowels
Stay Hydrated to Support Digestive Health
Aim for around 8 cups of fluid per day, spaced evenly throughout the day. Avoid caffeine after 12 pm if you struggle with sleep.
Improve How You Eat, Not Just What You Eat
The way you eat can make a big difference to bloating:
- Sit down for meals – don’t eat while standing up, walking or driving.
- Chew your food well and place your cutlery down between mouthfuls.
- Focus on what you’re eating – try to avoid eating while watching TV, scrolling on your phone, or doing both at the same time.
Boost Fibre Intake to Support Hormones and Gut Health
Focus on eating 5 portions of fruit and vegetables per day, choosing wholegrain varieties of cereals, and including beans, pulses, nuts, and seeds regularly in your diet. This will not only feed your gut microbiome, allowing it to produce beneficial short-chain fatty acids to keep your gut healthy and recycle your sex hormones, but it will also help reduce inflammation, the risk of heart disease, and certain cancers, as well as support weight management.
A Mediterranean diet has been shown to reduce hot flushes by up to 20% (3). With only 4% of the population getting the recommended 30 g of fibre per day (National Diet and Nutrition Survey: 2019–2023, reported June 2025 (4)), most of us have room to improve.

When increasing your fibre intake, do so slowly over a number of weeks to minimise the chances of worsening your bloating. If you’re struggling to increase fibre and experiencing painful, embarrassing digestive issues, you might need a more personalised approach that focuses on increasing the less fermentable fibres in your diet. You can contact me here to arrange a free discovery call.
Prioritise Quality Sleep to Reduce Gut Symptoms
Science tells us that even before perimenopause, poor sleep has a negative impact on our digestive health. I often advise my clients to use the 3–2–1 method to help improve sleep:
- 3 – Stop eating 3 hours before bed
- 2 – Stop drinking 2 hours before bed
- 1 – Stop screens 1 hour before bed
I also advise avoiding caffeine after 12 pm. Caffeine can remain in your system for up to 10 hours, and often, if your sleep is poor, your reliance on caffeine increases, which perpetuates the problem. Remember too that even drinks billed as “healthy” (matcha, I’m looking at you!) can contain as much caffeine as regular coffee.
Manage Stress to support Digestion
I appreciate that no one has ever become less stressed simply by being told to “be less stressed”, just as no one in the history of the world has calmed down by being told to “calm down”!
What I would urge you to do is put yourself first. You can’t care for others if your cup is half full. It’s a bit like when the flight attendant tells you to put on your own oxygen mask first.
As women, we’ve been conditioned to do for others first. I want you to know that you need to prioritise your own wellbeing – you do not need to earn it. Ever. (It’s something I’m working on too!)
Gentle movement to help ease bloating
Gentle activity, such as walking after meals, can help reduce bloating. Another helpful activity is yoga, which has been shown to be as beneficial as dietary changes, hypnotherapy, and medication in reducing IBS symptoms such as bloating, constipation, diarrhoea, and pain (5).
Bloating during perimenopause and menopause is common, but it isn’t something you just have to put up with. By understanding what’s happening in your body and making small, targeted changes to your diet, lifestyle, and routine, you can support your gut health and feel more like yourself again.
Whether it’s improving fibre intake, managing stress, focusing on sleep, or adjusting how you eat, even small steps can make a big difference to how your digestion feels day to day. If you’re struggling to pinpoint what’s causing your bloating or how to tackle it, getting tailored advice can help you make progress faster.
When to See a Doctor About Bloating
While bloating is very common during perimenopause and menopause and often improves with dietary and lifestyle changes, it’s important to know when it could be a sign of something more serious.
Contact your GP if you experience any of the following red flag symptoms:
-
Persistent or worsening bloating that doesn’t improve with simple changes
-
Unexplained weight loss or loss of appetite
-
Blood in your stool or black, tarry stools
-
Severe or ongoing abdominal pain
-
Changes in your bowel habits (such as new constipation or diarrhoea) that last more than a few weeks
-
Feeling full quickly or difficulty eating normal portions
These symptoms don’t always mean something serious is wrong, but they should be checked. Your GP can rule out other conditions, such as coeliac disease, inflammatory bowel disease, or, in rare cases, ovarian or bowel cancer and refer you for further investigation if needed.
If something doesn’t feel right, trust your instincts. It’s always worth speaking to your doctor rather than waiting and worrying.
If you feel that you have tried everything to help your bloating then why not download my Free Beat the Bloat Guide
If you’d like personalised support and a plan designed around your symptoms, you can book a free discovery call with me. Together, we’ll look at what’s going on with your gut, identify possible triggers, and build a strategy to help you feel comfortable and confident again.
If you have enjoyed this article then you might also like to read – What to eat for better gut health – A dietitians expert guide

Fiona Brannigan, BSc (Hons) Human Nutrition & Dietetics, HCPC-Registered Dietitian, Full member of the British Dietetic Association
Fiona Brannigan is a UK-registered dietitian and founder of Inspirit Nutrition & Dietetic Consultancy, based in Ayrshire and working with clients across the UK. With over 25 years of experience, including more than two decades in the NHS, Fiona has supported thousands of people to improve their health through nutrition.
Her expertise spans gut health, menopause nutrition, digestive disorders, neurological conditions, and rehabilitation following illness. Fiona is particularly passionate about helping adults aged 50+ regain confidence and control over their gut health, manage symptoms such as bloating, constipation, and diarrhoea, and enjoy food without fear or discomfort.
Fiona is regulated by the Health and Care Professions Council (HCPC) and is a member of the British Dietetic Association (BDA). She offers one-to-one consultations online and in person, using evidence-based nutrition and personalised support to help people feel their best at every stage of life.
Book a free discovery call to discuss your gut health goals or learn more about Fiona’s work


